May is Maternal Mental Health month. This month is meant to help raise awareness for maternal mental health while lifting the shame and stigma associated with these disorders.
There’s an unrealistic illusion that motherhood is a glowy, sparkly, precious cloud of bliss and light. Between movies and social media, new mothers are led to envision new motherhood as peaceful, beautiful, and picture-perfect—with lots of flowers, light streaming through the windows, and picture-perfect homes. They see mothers with dewy skin, glowing cheeks, perfect hair, and faces of angelic peace, bliss, and happiness and believe that’s the norm.
But it’s not.
Between sleepless nights, regular feedings, constant diaper changes, and fluctuating hormones—all piled on normal daily responsibilities—new motherhood is tough. It’s emotional, it’s stressful, and it’s messy.
And that’s normal. And it’s okay.
The destructive illusion of motherhood puts undue pressure and stress on mothers from all walks of life. But even more harmful is that this illusion creates a stigma that prevents mothers from seeking help when they need it most.
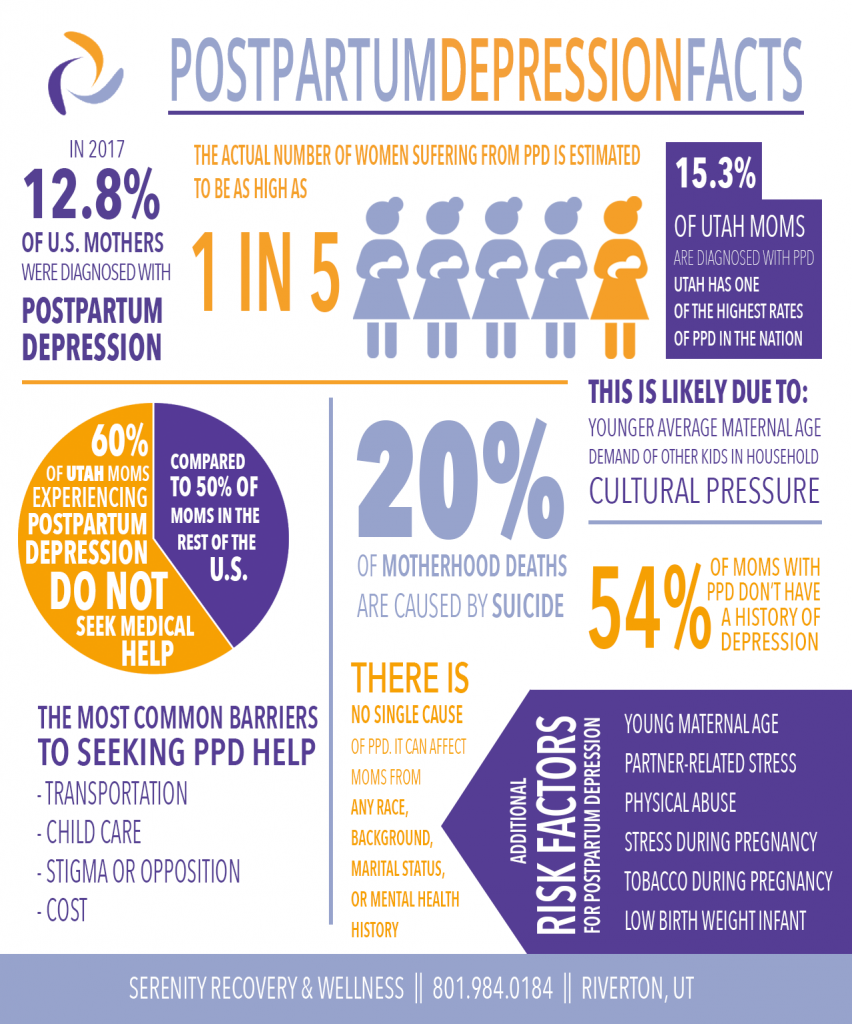
In 2017, there were over 500,000 diagnosed cases of postpartum depression. However, 66% of postpartum depression is never diagnosed. According to some reports, this likely puts the number closer to 900,000 cases per year in the U.S. However, although postpartum depression is highly treatable (with an 80%+ success rate in treatment), only 50% or fewer moms will actually seek medical treatment. One of the primary barriers to seeking help is stigma.
Below, we’ve shared statistics about postpartum depression in hopes of raising awareness for maternal health and to help lift the shame and stigma of postpartum depression.
How Common is Postpartum Depression?
- 12.8% of U.S. moms reported experiencing postpartum depression in 2018.
- That’s 1 in 8 moms.
- But that doesn’t take into account undiagnosed PPD, which is estimated to put the number closer to 20% of moms, or 1 in 5. It also doesn’t include PPOCD or postpartum psychosis.
- Which could mean as many as 790,000 U.S. women suffer from a perinatal mood or anxiety disorder in the U.S. each year.
- However, this number is only for live births and doesn’t take into account women who have miscarried or had a stillbirth. Taking this into consideration, the number is likely closer to 900,000 women annually in the U.S.
- 66% of PPD cases go undiagnosed. It is the most under-diagnosed obstetrical complication in the United States.
- Arkansas has the highest rate of postpartum depression with 22.3% of moms reporting experiencing PPD symptoms in 2018.
- Utah has among the highest rates of postpartum depression, with as many as 15.3% of moms reporting experiencing PPD symptoms.
What are the Risk Factors for Postpartum Depression?
- Only 54% of women experiencing PPD have been diagnosed with depression previously, either earlier in pregnancy or earlier in lifetime.
- Moms who have already experienced PPD have a 50% chance of experiencing it again in future pregnancies.
- Young moms (19 or younger) are 47% more likely to suffer from postpartum depression than moms over 25.
- Married moms are 65% less likely to experience PPD than moms with an unmarried relationship status.
- Moms suffering from physical abuse are 71% more likely to suffer from postpartum depression.
- 8% of mothers with preterm childbirths will suffer from postpartum depression.
- Pregnancy intention also affects postpartum depression, with more mothers who are “unsure” about pregnancy more likely to experience PPD than those who decidedly were or were not intending to get pregnant.
Other risk factors include:
- Partner relationship stress
- Traumatic or emotional stress during pregnancy
- Financial stress during pregnancy
- Tobacco use during pregnancy
- Delivery of low birthweight infant
- Not breastfeeding, or discontinuing breastfeeding before 6 months
Postpartum Depression Treatment Statistics
- On average, only 50% of US moms seek treatmentfor postpartum depression
- Postpartum depression is most often treated with a combination of medication and counseling.
- The most common barriers to treatment are:
- Cost
- Transportation
- Child care needs
- Stigma
- The overall success rate for treating postpartum depression is over 80%
When Postpartum Depression is Not Treated
- Suicide is the#2 cause of mortality for postpartum women, with 20% of deaths caused by suicide.
- 20% of moms still experience symptoms 1 year after childbirth.
- Children exposed to maternal depression are at higher risk of
- Delayed cognitive and language development
- Mental health problems
- Suboptimal physical growth
- Interpersonal, neuroendocrine, and behavioral problems
Utah Mother Postpartum Depression Statistics
Utah mothers are more likely to suffer from postpartum depression, and less likely to seek help:
- 8% of Utah moms were diagnosed with postpartum depression in 2017.
- That’s 3% higher than the national average.
- There were about 51,500 births in Utah last year, which means there were at least 8137 Utah mothersin 2017 alone who began suffering from postpartum depression.
- This is likely because Utah moms are often:
- Younger
- Have existing demands of raising other kids in the household
- Face cultural pressure
- 60% of Utah moms do not seek medical helpfor their postpartum depression (compared to 50% U.S. average).
- This is also likely due to cultural pressure and stigma, but can also be exacerbated by the need for childcare during treatments or opposing treatments
Sources
Centers for Disease Control and Prevention. “Depression Among Women.” https://www.cdc.gov/reproductivehealth/depression/index.htm. December, 2017.
Gentile S., Suicidal Mothers. J Inj Violence Res. 2011 Jul; 3(2): 90-97.
Public Health Indicator Based Information System (IBIS).Maternal and Infant Health Program, Division of Family Health and Preparedness, Utah Department of Health, Salt Lake City, UT. “Heath Indicator Report of Postpartum Depression.” Sep, 2016.
National Institute of Mental Heatlh. “Postpartum Depression Facts.” NIH Publication No. 13-8000. https://www.nimh.nih.gov/health/publications/postpartum-depression-facts/index.shtml
Ertel K., Rich-Edwards J., Koenen K., Maternal Depression in the United States: Nationally Representative Rates and Risks.J Womens Health. Larchmt. 2011 Nov; 20(11): 1609-1617
Postpartum Depression.org. “Postpartum Depression Statistics. https://www.nimh.nih.gov/health/publications/postpartum-depression-facts/index.shtml, 2017.
Katherine Stone, Postpartum Progress. “How Many Women Get Postpartum Depression? The Statistics on PPD.” http://www.postpartumprogress.com/how-many-women-get-postpartum-depression-the-statistics-on-ppd. October 2010.


